Spain: Multidrug-resistant bacteria found in 40% of meat samples in supermarkets

Antibiotic resistance is reaching dangerously high levels worldwide. Drug-resistant infections kill an estimated 700,000 people a year worldwide, and this figure is projected to rise to 10 million by 2050 if no action is taken. The World HEALTH Organization (WHO) classifies antibiotic resistance as one of the biggest threats to humanity.
Multidrug-resistant bacteria can be transmitted from animals to humans through the food chain, but due to commercial sensitivity, data on levels of antibiotic-resistant microbes in food are not widely available.
To learn more, Dr. Azucena Mora Gutiérrez and Dr. Vanesa García Menéndez of the University of Santiago de Compostela Lugo, Lugo, Spain, along with colleagues from other research centers, designed a series of experiments to assess levels of multidrug resistance in extraintestinal pathogens. enterobacteria (Klebsiella pneumoniae, E. coli and other bacteria that can cause multidrug-resistant infections such as sepsis or urinary tract infections) in MEAT sold in Spanish supermarkets.
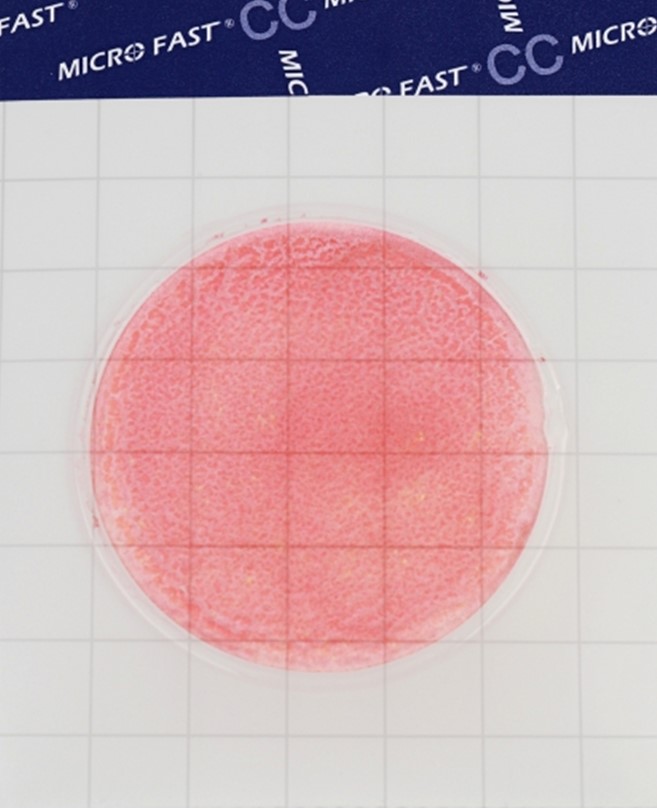
They analyzed 100 meat products (25 each from chicken, turkey, beef and pork) randomly selected from supermarkets in Oviedo during 2020.
Most (73%) meat products contained levels of E. coli that were within food safety limits.
Despite this, almost half (49%) also contained multiresistant and/or potentially pathogenic E. coli. Of these, 82 E. coli isolates were isolated and characterized. In addition, 12 K. pneumoniae isolates were isolated from 10 out of 100 meat products (7 from chicken, 2 from turkey, and 1 from pork).
Twenty-seven percent of meat products contained potentially pathogenic extraintestinal E. coli (ExPEC). ExPECs have genes that allow them to cause disease outside the gastrointestinal tract. ExPEC causes the vast majority of urinary tract infections (UTIs), is the leading cause of bacteremia (sepsis) in adults, and is the second most common cause of neonatal meningitis.
Six percent of meat products contained uropathogenic (UPEC) Escherichia coli – UPEC is part of the ExPEC group; they have specific virulence traits that allow them to cause UTIs.
One percent of meat products contained Escherichia coli with the mcr-1 gene. This gene confers resistance to colistin, the antibiotic of last resort used to treat infections caused by bacteria that are resistant to all other antibiotics.
The authors of the study , who in a previous study reported high levels of bacteria potentially capable of causing severe infections in humans, say their latest study shows that consumers can also be exposed to these bacteria through beef and pork .
They call for regular assessment of levels of antibiotic-resistant bacteria, including E. coli ExPEC, in meat products.
Dr Mora adds: “Intervening in the farm-to-table supply chain should be a priority to protect the consumer. For example, the introduction of laboratory surveillance methods to further study high-risk bacteria (in farm animals and meat) and their evolution in connection with the latest EU programs to limit the use of antibiotics in veterinary medicine. Farm-level strategies, such as vaccines, are needed to reduce the presence of specific multidrug-resistant and pathogenic bacteria in farm animals, which will reduce the risk of meat transportation and consumption.”
“The consumer plays a key role in food safety through proper food handling. Advice to consumers includes maintaining the cold chain from supermarket to home, cooking meat thoroughly, storing it properly in the refrigerator, and sanitizing knives, cutting boards, and other kitchen utensils used to prepare raw meat to avoid cross-contamination. With these measures, eating meat becomes a zero-risk pleasure,” adds the expert.